Total Hip Replacement
LOADING
Total Hip Replacement is one of the most successful operations of the 20th century, reliably restoring function, relieving pain, and returning mobility to literally tens of millions of patients around the planet since the early 1960’s, with a relatively low rate of serious complications.
Total Hip Replacement
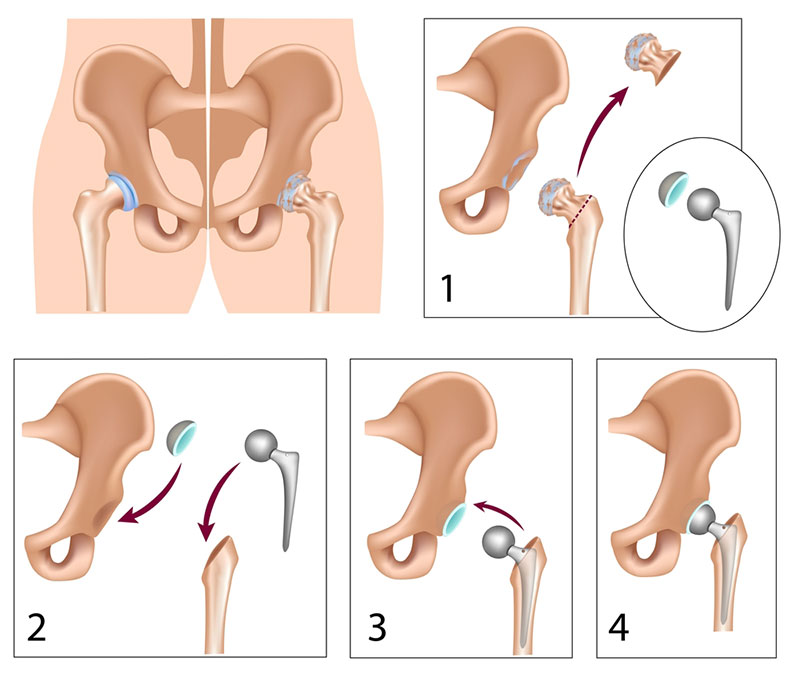
A total hip replacement is a major orthopaedic procedure, the aim of which is to remove the damaged/diseased portions of cartilage in both the upper part of the femoral neck and head as well as to resurface the inner cartilage lining of the acetabulum. On the femoral side, after removing the femoral head and neck, the neck is essentially replaced with a man-made metal stem which is implanted into the bone marrow of the upper femur (the femoral component). The stem then has a ball lodged on the top to replace the ball of the femoral head. The ball can be made of a number of different materials including a cobalt-chrome alloy, ceramic, or oxidised zirconium. On the acetabular side, the damaged/diseased cartilage of the socket of the acetabulum is burred away to leave a fresh bed of bone, into which a man-made acetabular shell is implanted. The shell can be made purely of a plastic material called polyethylene (and this requires the use of bone cement to bond it to the patients pelvic bone – see below), or alternatively it can have a metal outer backing called a “shell”, which requires the use of an inner liner that is then locked into the shell. The liner can be made from polyethylene (similar to the cemented version but without the need for the cement – see below), metal (e.g. cobalt-chrome alloy) which is used much less frequently in current trends, or ceramic. Thus, the moving parts of the hip replacement are the femoral head (the new ball) which rolls about in the acetabular component or its liner if it has one (the new socket).
The choice of what kind of hip replacement can also be broken down into two broad categories, based on how the implants become fixed or integrated into the bone and the patient’s body. The original technique (from the 1960’s) of bonding a hip prosthesis to the bone was described as a cemented hip replacement and required the surface of the bone to be coated with a 2-3mm thick layer of synthetic bone cement (PMMA – poly methyl methacrylate). This cement acts as a grout between the bone and the prostheses. It’s not an adhesive and doesn’t “glue” the implants to the bone – it merely fills any voids and ensures that the implants have as much contact with the bone as possible, stopping them from moving within the bone and providing a strong initial grip on the implants, which usually results in a painless bond between the implant and the bone. Alternatively, in an uncemented hip replacement, the implants themselves may be coated with a microscopically thin layer of synthetic chemical which attracts the patient’s own bone to grow directly onto the surface, or even into microscopic pores that have been manufactured onto the roughened surface of the implants, thus achieving an intimate bond directly between the patient’s bone and the implant.
It is also possible in some circumstances to mix and match, for instance in one patient a surgeon may implant a femoral component that is designed to be used with bone cement while the acetabular component may be uncemented. Vice versa is also possible too. Again, each of these design philosophies have their pros and cons that frequently cause debate within the orthopaedic communities around the globe as to which combination is preferable in which kinds of patient. Again, the fact that there is no overall consensus should indicate that there is no clear “winner” in this argument, and is frequently a case of “horses for courses” and which type of total hip replacement that the surgeon is most comfortable and familiar with to give the most reliable and predictable outcomes for their patients.
The total hip replacement can be performed by entering the hip joint using any one of a number of different pathways through the muscles about the hip, known as an “approach”. There is no single “best” approach to the hip for all patients, or for all surgeons or for all hip procedures– each approach has its own unique advantages and disadvantages with respect to numerous factors such as:
An alternative bearing combination is a ceramic femoral head and a ceramic acetabular liner. The advantage of this combination is that it has been thought (up until recently) to have the slowest rates of wear out and thus the least amount of inflammatory debris formation. It is thus anticipated that it would be the most durable, most inert combination of moving parts that would last the patient for most of their lifetime. While this is frequently the case, in the past, the ceramic used has been much more brittle than the metal or polyethylene components, and so if a sudden force has been applied to the hip – e.g. landing after a heavy jump, in very rare cases the ceramics can either crack, chip or shatter, similar to how a ceramic cup might if you dropped a ceramic plate on top of it. Fortunately, this is very uncommon, but if it does occur it is a serious and major problem to resolve.
In most recent years, a unique new material called Oxinium has been manufactured and used for the femoral head, in combination with a polyethylene acetabular liner. This combination has the advantage (so far) in demonstrating rates of wearing out that are similar if not slightly better than a ceramic-ceramic bearing couple, but without the brittleness of an acetabular liner, and thus a much smaller risk of fracture. Unfortunately, being a new substance, no-one can accurately predict what will happen in the future to total hip replacements using this combination of bearings, although to date the trend appears promising.
If you are reading this section, then it’s probable that you would already be aware of the controversy regarding the use of “metal-on-metal” total hip replacements. With this combination, both the femoral head, and the liner that sits within the acetabular shell are made out of an alloy of cobalt and chrome. The trend towards using a metal-on-metal combination of components is largely declining as this has been associated with a higher than expected (and tolerated) rate of the components wearing out requiring revision surgery. There have been a few notable brands of total hip replacements, such as the “ASR hip”, that fall into this category of large metal-on-metal total hip replacements that have performed poorly due to the combination of bearing surfaces.
Again, each of these bearing couples have their “pros” and “cons” that need to be tailored to the activity level and expectations of the patients and the surgeons level of familiarity.
Total hip replacement can be performed for end-stage arthritis of the hip which may have resulted from a wide variety of underlying condition such as:
Cemented vs Uncemented Total Hip Replacement
The choice of what kind of hip replacement can also be broken down into two broad categories, based on how the implants become fixed or integrated into the bone and the patient’s body. The original technique (from the 1960’s) of bonding a hip prosthesis to the bone was described as a cemented hip replacement and required the surface of the bone to be coated with a 2-3mm thick layer of synthetic bone cement (PMMA – poly methyl methacrylate). This cement acts as a grout between the bone and the prostheses. It’s not an adhesive and doesn’t “glue” the implants to the bone – it merely fills any voids and ensures that the implants have as much contact with the bone as possible, stopping them from moving within the bone and providing a strong initial grip on the implants, which usually results in a painless bond between the implant and the bone. Alternatively, in an uncemented hip replacement, the implants themselves may be coated with a microscopically thin layer of synthetic chemical which attracts the patient’s own bone to grow directly onto the surface, or even into microscopic pores that have been manufactured onto the roughened surface of the implants, thus achieving an intimate bond directly between the patient’s bone and the implant.
It is also possible in some circumstances to mix and match, for instance in one patient a surgeon may implant a femoral component that is designed to be used with bone cement while the acetabular component may be uncemented. Vice versa is also possible too. Again, each of these design philosophies have their pros and cons that frequently cause debate within the orthopaedic communities around the globe as to which combination is preferable in which kinds of patient. Again, the fact that there is no overall consensus should indicate that there is no clear “winner” in this argument, and is frequently a case of “horses for courses” and which type of total hip replacement that the surgeon is most comfortable and familiar with to give the most reliable and predictable outcomes for their patients.
Which “approach” is best for my total hip replacement?
The total hip replacement can be performed by entering the hip joint using any one of a number of different pathways through the muscles about the hip, known as an “approach”. There is no single “best” approach to the hip for all patients, or for all surgeons or for all hip procedures– each approach has its own unique advantages and disadvantages with respect to numerous factors such as:
- the size and location of the incision
- the cosmetic appearance of this incision
- prospective damage to muscles and tendons
- risk to damaging nearby nerves and arteries
- the ability for the surgeon to assess the tension in the muscles acting around and the stability of the prosthetic hip joint – also known as the risk of dislocation
- the ability to get adequate visualisation of all the structures required to safely perform the various steps of the surgery, and consequently the ability to implant the prosthetic components in the best orientation or position to achieve an excellent fit within the bones and with the optimal orientation to provide a stable, secure prosthetic hip joint
- the ability to obtain a more extensive field of surgery which may be required to deal with more complicated cases, unusual anatomy or any potential complications that may occur during surgery
- the ability to be used in patients of various body shapes and sizes
Which moving parts are best?
Finally, another factor in considering “what type of hip replacement” is going to be used is “what should the moving parts of the hip replacement be made of?” Probably the most frequently seen combination is a cobalt-chrome femoral head articulating with a polyethylene acetabular liner (“metal-on-poly”). This combination has, with the original types of polyethylene, been associated with cases of late destruction of the patient’s bone, 10 or more years after the initial surgery. This has been due to microscopic amounts of polyethylene debris (“wear particles”) being generated which cause inflammation around the hip joint, and the inflammation then drives the destructive process, resulting in breakdown of otherwise previously healthy bone in a process called “osteolysis”. It is thought that with newer versions of polyethylene this should happen either less frequently, or much later on in the lifespan of the total hip replacement, and that osteolysis will be much less commonly seen with the newer polyethylenes. These have been available over the past 7-10 years approximately.An alternative bearing combination is a ceramic femoral head and a ceramic acetabular liner. The advantage of this combination is that it has been thought (up until recently) to have the slowest rates of wear out and thus the least amount of inflammatory debris formation. It is thus anticipated that it would be the most durable, most inert combination of moving parts that would last the patient for most of their lifetime. While this is frequently the case, in the past, the ceramic used has been much more brittle than the metal or polyethylene components, and so if a sudden force has been applied to the hip – e.g. landing after a heavy jump, in very rare cases the ceramics can either crack, chip or shatter, similar to how a ceramic cup might if you dropped a ceramic plate on top of it. Fortunately, this is very uncommon, but if it does occur it is a serious and major problem to resolve.
In most recent years, a unique new material called Oxinium has been manufactured and used for the femoral head, in combination with a polyethylene acetabular liner. This combination has the advantage (so far) in demonstrating rates of wearing out that are similar if not slightly better than a ceramic-ceramic bearing couple, but without the brittleness of an acetabular liner, and thus a much smaller risk of fracture. Unfortunately, being a new substance, no-one can accurately predict what will happen in the future to total hip replacements using this combination of bearings, although to date the trend appears promising.
If you are reading this section, then it’s probable that you would already be aware of the controversy regarding the use of “metal-on-metal” total hip replacements. With this combination, both the femoral head, and the liner that sits within the acetabular shell are made out of an alloy of cobalt and chrome. The trend towards using a metal-on-metal combination of components is largely declining as this has been associated with a higher than expected (and tolerated) rate of the components wearing out requiring revision surgery. There have been a few notable brands of total hip replacements, such as the “ASR hip”, that fall into this category of large metal-on-metal total hip replacements that have performed poorly due to the combination of bearing surfaces.
Again, each of these bearing couples have their “pros” and “cons” that need to be tailored to the activity level and expectations of the patients and the surgeons level of familiarity.
Total hip replacement can be performed for end-stage arthritis of the hip which may have resulted from a wide variety of underlying condition such as:
- Osteoarthritis (possibly due to FAI),
- Inflammatory arthritis, (e.g. Rheumatoid Arthritis, Psoriatic Arthritis, SLE, Juvenile Chronic Arthritis)
- Treated septic arthritis (i.e. an infection of the hip joint many years ago has been treated so that the infective microbes no longer exists, but the cartilage has been severely damaged during the infection)
- Secondary to hip dysplasia (see section on hip dysplasia)
- Post-traumatic arthritis (i.e. after motor vehicle trauma or serious sporting injuries, where the acetabulum or femoral head may have healed poorly (or not at all) after a fracture)
- Avascular necrosis of the femoral head – a condition which may occur for a number of reasons, the end result being a blockage of blood flow to the head of the femur which causes the bone in that region to collapse with subsequent loss of cartilage.
The information above is general. All surgical procedures involve some risk. If you would like advice on your specific condition, please contact the office of Mr Daniel Robin, Melbourne Orthopaedic Surgeon.

